Massive Multinodular Goiter With Retrosternal Extension in a Patient With Long-Standing Thyroid Disease
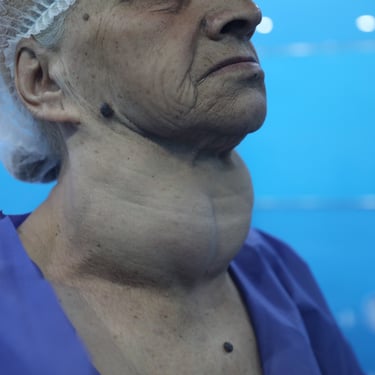
A middle-aged patient presented with progressive neck swelling accompanied by difficulty swallowing. He had a 10-year history of thyroid disease, along with hypertension and heart disease. His medication regimen included carbimazole 5 mg, propranolol, concor 10 mg, and torsicalm. He reported no previous surgeries, had no known drug allergies, and denied any recent flu-like symptoms. He was a passive smoker. The chronicity of symptoms and the presence of compressive manifestations suggested a large, slowly enlarging goiter likely related to long-standing structural thyroid disease.
SURGERYHEAD AND NECKVIDEO
12/2/20252 min read


Patient Presentation:
A middle-aged patient presented with progressive neck swelling accompanied by difficulty swallowing. He had a 10-year history of thyroid disease, along with hypertension and heart disease. His medication regimen included carbimazole 5 mg, propranolol, concor 10 mg, and torsicalm. He reported no previous surgeries, had no known drug allergies, and denied any recent flu-like symptoms. He was a passive smoker. The chronicity of symptoms and the presence of compressive manifestations suggested a large, slowly enlarging goiter likely related to long-standing structural thyroid disease.
Laboratory Investigations:
Laboratory evaluation showed a TSH level of 1.57 uIU/mL and an FT4 level of 8.54 pmol/L, indicating a near-euthyroid or mildly hypothyroid pattern. TSH receptor antibody (TRAb) was <0.800 IU/L, not suggestive of Graves disease. Preoperative testing revealed markedly elevated thyroglobulin (>500 ng/mL), consistent with extensive multinodular goiter tissue burden. Serum calcium was normal at 10.0 mg/dL. Overall, the biochemical profile aligned with a large multinodular goiter rather than autoimmune disease or hyperthyroidism.
Ultrasound Findings:
Ultrasound examination of the thyroid demonstrated marked bilateral enlargement. The right lobe measured 150 × 85 × 71 mm and the left lobe 140 × 83 × 50 mm, with an isthmus thickness of 20 mm. The gland displayed heterogeneous echotexture and contained multiple well-defined nodules of variable size. The largest nodules measured 47 × 40 × 39 mm in the right lobe and 55 × 44 × 40 mm in the left lobe, both classified as TR3. Mildly increased vascularity was noted, and macrocalcifications were present in some nodules. Bilateral retrosternal extension was also seen on ultrasound. These findings were strongly suggestive of a massive multinodular goiter with potential compressive sequelae.
CT Neck and Chest Findings:
CT imaging of the neck, base of skull, and upper chest confirmed significant enlargement of both thyroid lobes and the isthmus. The right lobe measured 130 × 80 × 63 mm and the left lobe 100 × 70 × 65 mm, with an isthmus of 68 × 20 mm. The enlarged gland formed a dominant anterior neck mass with components extending posterior to the trachea. Both lobes demonstrated heterogeneous density with multiple nodules, calcifications, and areas of cystic degeneration. Marked retrosternal extension was present, reaching down near the level of the tracheal carina. Additionally, diffuse heterogenous vertebral bone density with small hypodense areas was noted, warranting follow-up to rule out pathological lesions, although no direct association with the thyroid pathology was clear at the time.
Surgical Management:
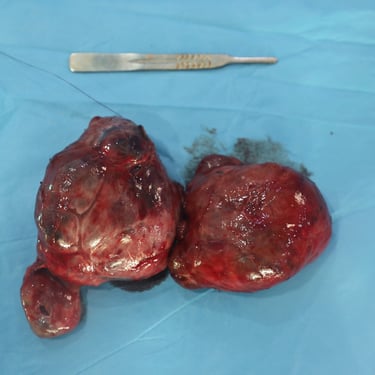
Given the large multinodular goiter with retrosternal extension, compressive symptoms, and the risk of further progression, surgical intervention was planned. The patient underwent thyroidectomy following standard preoperative assessment, which was notable for the high thyroglobulin level but otherwise unremarkable metabolic status. Intraoperative findings were consistent with a massive bilateral goiter with deep mediastinal descent.
Histopathological Examination:
Histopathology revealed thyroid follicular nodular disease with benign secondary changes, confirming the diagnosis of multinodular goiter. No evidence of malignancy was identified. The pathology matched imaging expectations for long-standing benign nodular hyperplasia.
Postoperative Course and Follow-Up:
The patient had a smooth postoperative recovery without significant complications. Airway symptoms improved, and no major issues such as hypocalcemia or nerve injury were reported. He was discharged with follow-up recommendations for thyroid hormone replacement and long-term surveillance, particularly given the pre-existing vertebral imaging abnormalities requiring future reevaluation.